Hey, everyone! Long time no blog. ![]() Between moving, and studying for (and writing) the Canadian Society for Medical Laboratory Science certification exam, I haven’t had much time to gather my thoughts. Though I’ve started working as a tech now, I wanted to touch on a few topics I missed before practicum finished.
Between moving, and studying for (and writing) the Canadian Society for Medical Laboratory Science certification exam, I haven’t had much time to gather my thoughts. Though I’ve started working as a tech now, I wanted to touch on a few topics I missed before practicum finished.
My last 6 weeks were spent in Transfusion Medicine, a.k.a. blood bank – the department responsible for the testing and issuing of blood and blood components.
Whole blood is comprised of red blood cells, plasma, and a buffy coat (white blood cells and platelets). A and B antigens are found on the surface of RBCs, with their presence/absence designating a person’s blood group. These antigens can bind to and cause severe reactions with their corresponding antibodies, which are found in plasma. Fortunately, our bodies produce antibodies against only the A and B antigens we do not have on our red cells.
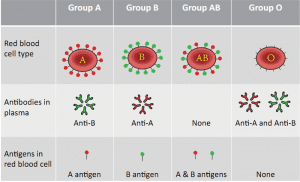
If we only make antibodies to the ABO antigens we don’t have, when might a reaction occur? Think about this: can a Group A individual be safely transfused with AB red cells?
Matching an individual’s blood type with that of the blood to be transfused is imperative in preventing transfusion reactions and maximizing survival of the RBCs.
Be the first to receive the latest BCIT News. Become a subscriber.
Blood samples are collected prior to anticipated transfusions (e.g. surgery) for ABO/Rh typing and an antibody screen. The most important antigen in the Rh blood group system is D; observed in conjunction with an ABO group, O+ (positive) individuals have the D antigen on their red cells, and O– (negative) individuals do not. Unlike the naturally occurring antibodies of the ABO system, Rh antibodies only develop in Rh- individuals after exposure to Rh+ cells—such as Rh+ fetal cells crossing the placenta into an Rh- mom’s circulation at birth.
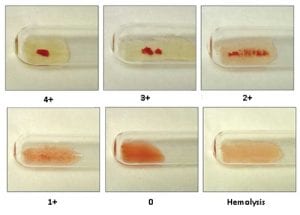
ABO/Rh typing involves combining either a) patient red cells with antisera containing antibodies against A, B, or D antigens, or b) patient plasma with A1 or B reagent red cells (there is no reverse grouping for D as per the reasons above). Clumping, or agglutination, indicates a positive reaction.
An antibody screen is used to screen for antibodies against antigens of non-ABO blood group systems. There are over 30 recognized blood group systems; some of the important ones which can be tested for in the lab are the Kell, Duffy, Kidd, and MNS systems.
Patient plasma is tested against 2 or 3 Group O screening cells—which will not have potentially interfering A or B antigens, but will have varying combinations of antigens which may be the target of significant antibodies within other blood group systems. If the screen is positive, further testing must be done to identify the antibody/antibodies before the sample can be crossmatched with donor units negative for the corresponding antigen(s). This is one of the final compatibility checks performed in the lab.
Transfusion Medicine can feel like a slower-paced department, but don’t be mistaken—one should be prepared to handle the stress of a massive transfusion protocol at all times (be forewarned, that web page is not a light read!). My trainers described it as ‘feast or famine’ and, though graphic, it’s a valid comparison.
Learn more about the Medical Laboratory Science full-time diploma program at BCIT.
Hello Natalie,
I am a current Med Lab Science student at BCIT. I’m starting Level 2 in September 2019. I’ve thoroughly enjoyed your postings to the point I’ve read them all in one sitting. This really helped me visualize how the long practicum term would be for a student. Plus it honestly, reinforced my thoughts about how passionate I am about this career. Thank you very much for your insight and congratulations on starting work as a Med Lab Tech !!!
Hi Pavi, thank you so much for taking the time to read my blog! I’m glad you found it even the slightest bit useful, and that you’re passionate and excited about where this career will take you. Best of luck as you continue your journey at BCIT & beyond!