As promised in my last blog, here’s a case study that more or less mimics the thought process of a technologist on the Hematology bench.
The CBC analyzer flags a platelet count of 67 x 109/L (the normal reference range is 150-450 x 109/L). It is the first time this patient’s platelet count has dropped below 100 x 109/L, and so a platelet estimate is ordered.
There are several reasons a platelet count could be decreased. Poor mixing, difficult collection, and EDTA-induced platelet clumping (pseudothrombocytopenia) are in vitro phenomena – sometimes related to sample collection, but never of physiological significance. In vivo causes (occurring within the body and of potential significance) include pancytopenia, which presents with decreased platelets, WBCs, and RBCs; if the patient is post-operative or undergoing chemotherapy; disseminated intravascular coagulation (DIC) – a condition characterized by the obstruction of smaller blood vessels by overactive clot formation. This leads to increased consumption of clotting factors and platelets, and increased risk of a serious bleed.
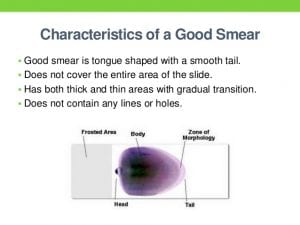
You scan the stained smear, first examining the feathered edge (tail) and margins for platelet clumps. Clumping mimics a low platelet count as the analyzer is unable to differentiate a clump from an individual cell; if present, they are usually most abundant in these areas. You also do not see any platelet satellitism—associated with EDTA-induced clumping, hence that is unlikely to be the cause.
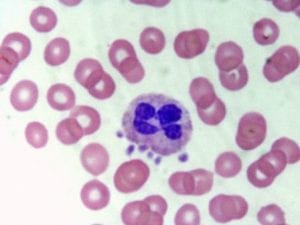
You count the platelets in several fields, take the average, and multiply it by your facility’s platelet factor. The result is close to 67 x 109/L, so you have verified that the platelet count is, truly, decreased.
Are you a BCIT News insider? Sign-up to receive the latest news on BCIT.
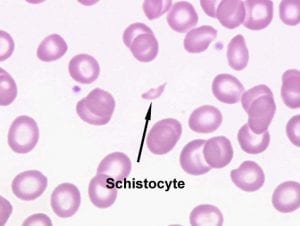
Only a platelet estimate was ordered in this scenario, but it is quality practice to keep all cell types in mind when examining a slide. Abnormal red cell morphology like schistocytes are sometimes seen in patients with DIC.
Let’s say you observe and grade 1+ schistocytes.
You’re almost done! Long-time technologists have the criteria memorized—if not, refer to your facility’s job aid on when to send a slide to a pathologist. If it says to refer the presence of 1+ schistocytes in conjunction with a platelet count of ˂ 100 x 109/L the slide is referred, unless the patient already has a pathologist comment addressing these atypical findings. (Such a comment would be found in the patient’s clinical history—remember what I said about looking into past results?) Just like technologists in the lab, pathologists too have a heavy workload; you wouldn’t want to give them a case that has already been assessed.
Phew, that was a lot of words stemming from a platelet count of 67 x 109/L! It goes to show how much thought can go into a single specimen—and how with experience, technologists build up the muscle memory to work through many more with efficiency.
Interested in the Medical Laboratory Science full-time diploma program? Join the next online info session at BCIT.
